8 Powerful Facts About Human Herpesviruses: Complete Guide with Diagnosis & Prevention
Ultimate Guide: Classification, Clinical Features, Diagnosis, Treatment, and Prevention of Human Herpesviruses
General Properties Human Herpesviruses
- DNA enveloped virus
- Double-stranded linear DNA
- Envelope obtained by budding from the nuclear membrane
- Icosahedral nucleocapsid
- Forms giant cells and intranuclear inclusion bodies
- Can cause lifelong latent infections with reactivation
Structure of Herpesvirus Virion
- Glycoproteins
- Capsid
- Envelope
- DNA
- Tegument
Herpesvirus Classification and Characteristics
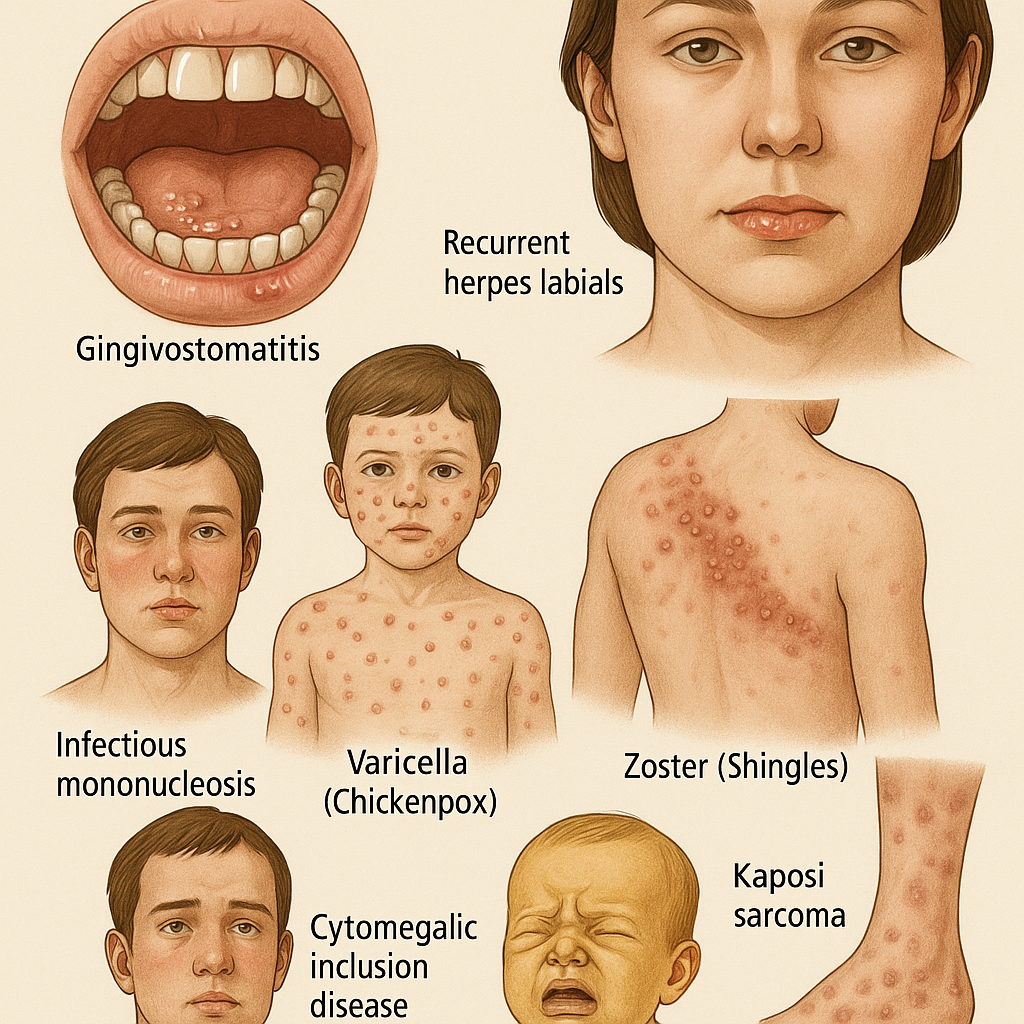
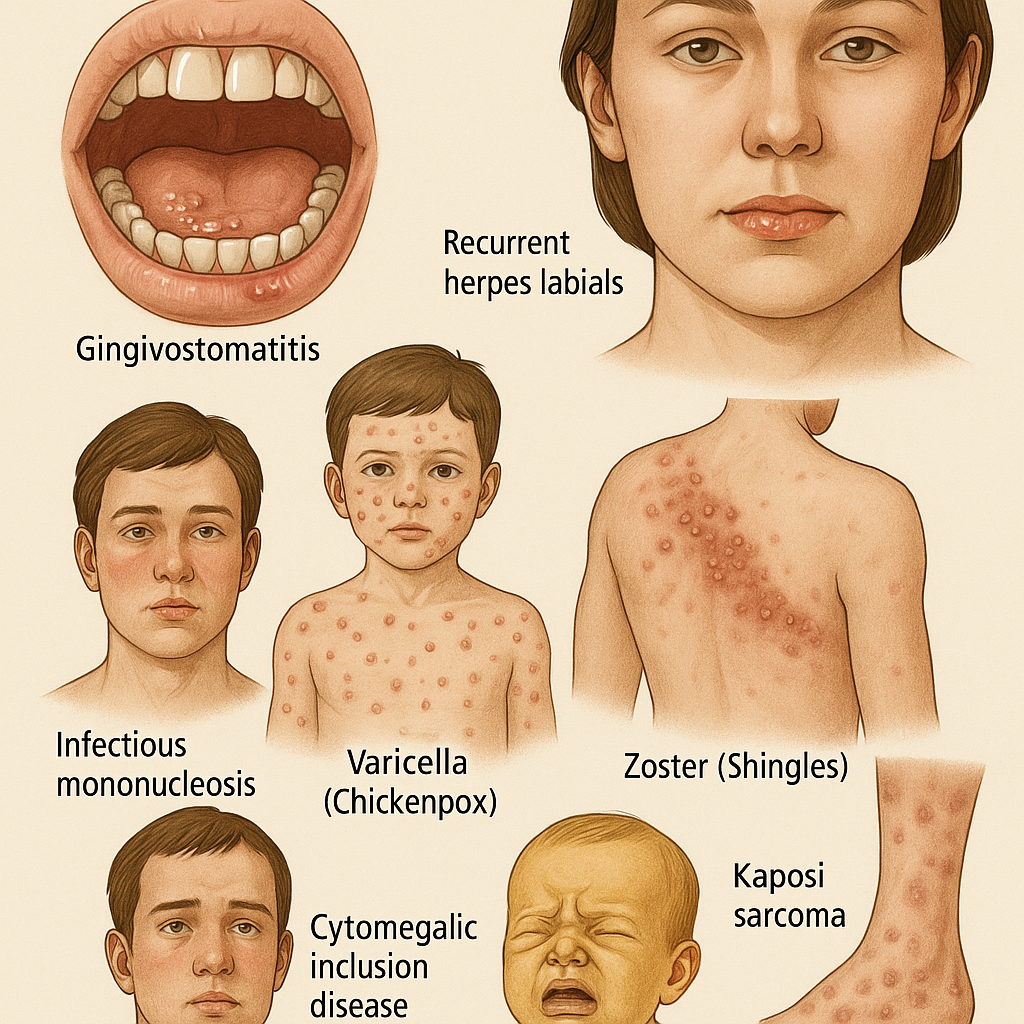
| HSV-1 / HHV-1 | Mucoepithelial cells | Respiratory secretions, saliva | Gingivostomatitis, herpes labialis, keratoconjunctivitis, encephalitis | Trigeminal ganglia |
| HSV-2 / HHV-2 | Mucoepithelial cells | Sexual contact, perinatal infection | Genital herpes, neonatal herpes, aseptic meningitis | Lumbar and sacral ganglia |
| HHV-3 / VZV | Mucoepithelial cells | Respiratory secretions | Varicella (chickenpox), herpes zoster (shingles) | Thoracic sensory ganglia |
| HHV-4 / EBV | B cells | Respiratory secretions, saliva | Infectious mononucleosis, Burkitt’s lymphoma, B cell lymphoma, nasopharyngeal carcinoma, hairy leukoplakia | Lymphoid tissue |
| HHV-5 / CMV | Monocytes, lymphocytes, epithelial cells | Transfusion, sexual contact, congenital | Mononucleosis, CMV inclusion disease in neonates, pneumonia in immunocompromised | Glands, kidneys |
| HHV-6 | T cells | Respiratory secretions | Roseola (exanthem subitum) | Lymphoid tissue |
| HHV-7 | T cells | Respiratory secretions | Not linked to any specific disease | Lymphoid tissue |
| HHV-8 | Endothelial cells | Sexual contact, organ transplantation | Kaposi’s sarcoma, mononucleosis-like syndrome | Vascular endothelium |
HSV-1 vs HSV-2 Characteristics
| Feature | HSV-1 | HSV-2 |
|---|---|---|
| Transmission | Saliva | Sexual contact |
| Diseases | Cold sores, keratitis, encephalitis | Genital herpes, neonatal herpes, aseptic meningitis |
| Lesion location | Above the waist | Below the waist |
| Latency | Trigeminal ganglia | Lumbar/sacral ganglia |
HSV Pathogenesis
After initial replication in skin or mucous membranes, the virus travels via retrograde axonal transport to the sensory ganglia where it establishes latency. Reactivation is triggered by sunlight, hormonal changes, trauma, stress, or fever.
Laboratory Diagnosis
- Tzanck smear: Multinucleated giant cells on Giemsa stain
- Virus isolation: Cell culture, fluorescent antibody staining
- Serological tests: IgM detection, ELISA, latex agglutination
- Nucleic acid tests: PCR, especially useful for encephalitis diagnosis
Treatment
- Acyclovir – Encephalitis, systemic HSV-1, genital HSV-2
- Trifluridine – HSV-1 eye infection
- Penciclovir – Recurrent oral HSV-1
- Valacyclovir, Famciclovir – Genital herpes, recurrence suppression
Prevention
- No vaccine currently available
- Antivirals can reduce recurrence and shedding
- Cesarean delivery recommended for infected pregnant women at term
- Circumcision reduces HSV-2 risk
Varicella Zoster Virus (VZV)
- Primary Disease: Varicella (Chickenpox)
- Recurrent Form: Zoster (Shingles)
- Single serotype
- Humans are the natural host
Varicella Zoster Virus (VZV)
- Primary Disease: Varicella (Chickenpox)
- Recurrent Form: Zoster (Shingles)
- Single serotype
- Humans are the natural host
Transmission
- Respiratory droplets
- Direct contact with lesions
- Varicella is a highly contagious disease of childhood
Pathogenesis of Varicella
- Infection begins in the mucosa of the upper respiratory tract (URT)
- Initial replication occurs in regional lymph nodes
- Primary viremia spreads virus to liver and spleen for further replication
- Secondary viremia involving infected mononuclear cells transports virus to the skin
- Rash forms due to ballooning degeneration and fluid accumulation in epithelial cells
VZV infection and spread are limited by humoral and cell-mediated immunity, and interferons. Virus becomes latent in the dorsal root ganglia.
Pathogenesis of Zoster
- Reactivation occurs during reduced immunity or local trauma
- Replication in sensory nerve ganglia causes acute inflammation and pain
- Lesion distribution corresponds to the innervation of affected ganglia
- Virus travels to the skin via nerve fibers, forming vesicles
Clinical Features of Varicella
- Fever and malaise are early symptoms
- Rash appears first on trunk, then face, limbs, buccal and pharyngeal mucosa
- Rash progresses from macule → papule → vesicle → pustule → scab
- Rash lasts about 5 days; most children develop hundreds of skin lesions
Complications of Varicella
- Pneumonia (common)
- Post-viral encephalitis
- Hemorrhagic (fulminant) encephalitis
- Disseminated intravascular coagulation (DIC)
Clinical Features of Zoster
- Severe localized pain before rash
- Vesicles appear over skin area supplied by affected nerve
- Trunk, head, and neck are most commonly affected
- Ophthalmic division of trigeminal nerve involved in 10-15% of cases
Complications of Zoster
- Postherpetic neuralgia
- Keratoconjunctivitis
- Pneumonia
Laboratory Diagnosis
- Specimen: Vesicle fluid from the base of lesions
- PCR Test: Detects viral DNA; DFA also used on skin lesions
- Microscopy: Tzanck smear shows multinucleated giant cells
- Culture: Human embryonic kidney cells (3-7 days)
- Identification:
- Direct fluorescent antibody test
- Neutralization test
Prevention
In Bangladesh
- Varicella vaccine (Varilrix), 0.5 ml subcutaneously
- Children (1–12 years): 2 doses, 6 weeks apart
- Adults (>12 years): 2 doses, 6 weeks apart
- Live attenuated vaccine
In the Western World
- Varivax: Live attenuated vaccine to prevent varicella, recommended for those >12 months
- Shingrix: Recombinant glycoprotein E vaccine to prevent zoster, effective at any adult age
Additional Prophylaxis
- Acyclovir: Prevents varicella and disseminated zoster in immunocompromised individuals
- Varicella Zoster Immunoglobulin (VZIG): Used for prophylaxis post-exposure
Epstein-Barr Virus (EBV)
- Target Cells: B lymphocytes
- Site of Latency: Lymphoid tissue
Diseases Caused by EBV
- Infectious mononucleosis
- Tumors:
- Burkitt’s lymphoma
- Nasopharyngeal carcinoma
- Hodgkin’s disease and other B-cell lymphomas
- Oral hairy leukoplakia (in AIDS patients)
- Post-transplant lymphoproliferative disorder (PTLD)
- Hemophagocytic lymphohistiocytosis (HLH)
Antigenic Structure
- Viral Capsid Antigen (VCA) – used in diagnosis
- Early Antigen (EA) – produced before DNA synthesis
- Epstein-Barr Nuclear Antigen (EBNA) – found in the nucleus
- Viral Membrane Antigens
Transmission
- Exchange of saliva (kissing)
- Respiratory droplets
Pathogenesis
- Initial infection in oropharynx → bloodstream
- Infects B lymphocytes → Cytotoxic T cells attack infected cells
- Latency established in B cells
Laboratory Diagnosis
- Serological Tests:
- IgM VCA Ab → Acute infection
- IgG VCA Ab → Past infection
- EBNA and EA antibodies are also diagnostically useful
- Monospot test (heterophil Ab test): No longer recommended by CDC due to false results
- Peripheral Blood Film (PBF):
- Absolute lymphocytosis
- 30% atypical lymphocytes with lobulated nuclei and basophilic cytoplasm
- PCR: Detect viral DNA in blood
Treatment and Prevention
- No specific antiviral treatment for uncomplicated cases
- No vaccine available
Epstein-Barr Virus (EBV)
- Target Cells: B lymphocytes
- Site of Latency: Lymphoid tissue
Diseases Caused by EBV
- Infectious mononucleosis
- Tumors:
- Burkitt’s lymphoma
- Nasopharyngeal carcinoma
- Hodgkin’s disease and other B-cell lymphomas
- Oral hairy leukoplakia (in AIDS patients)
- Post-transplant lymphoproliferative disorder (PTLD)
- Hemophagocytic lymphohistiocytosis (HLH)
Antigenic Structure
- Viral Capsid Antigen (VCA) – used in diagnosis
- Early Antigen (EA) – produced before DNA synthesis
- Epstein-Barr Nuclear Antigen (EBNA) – found in the nucleus
- Viral Membrane Antigens
Transmission
- Exchange of saliva (kissing)
- Respiratory droplets
Pathogenesis
- Initial infection in oropharynx → bloodstream
- Infects B lymphocytes → Cytotoxic T cells attack infected cells
- Latency established in B cells
Laboratory Diagnosis
- Serological Tests:
- IgM VCA Ab → Acute infection
- IgG VCA Ab → Past infection
- EBNA and EA antibodies are also diagnostically useful
- Monospot test (heterophil Ab test): No longer recommended by CDC due to false results
- Peripheral Blood Film (PBF):
- Absolute lymphocytosis
- 30% atypical lymphocytes with lobulated nuclei and basophilic cytoplasm
- PCR: Detect viral DNA in blood
Treatment and Prevention
- No specific antiviral treatment for uncomplicated cases
- No vaccine available
Cytomegalovirus (CMV)
Transmission
- Close contact with secretions (saliva, respiratory)
- Blood transfusion
- Transplacental, delivery, breast milk
At-Risk Groups
- Organ transplant recipients
- Chemotherapy patients
- Immunocompromised individuals (e.g., AIDS)
- Fetuses
Diseases Caused by CMV
- Congenital cytomegalic inclusion disease in neonates
- Subclinical or asymptomatic infection in healthy individuals
- Renal issues in kidney transplant recipients
- Hepatitis post-liver transplant
- Graft atherosclerosis in heart transplant patients
- Interstitial pneumonia after bone marrow transplant
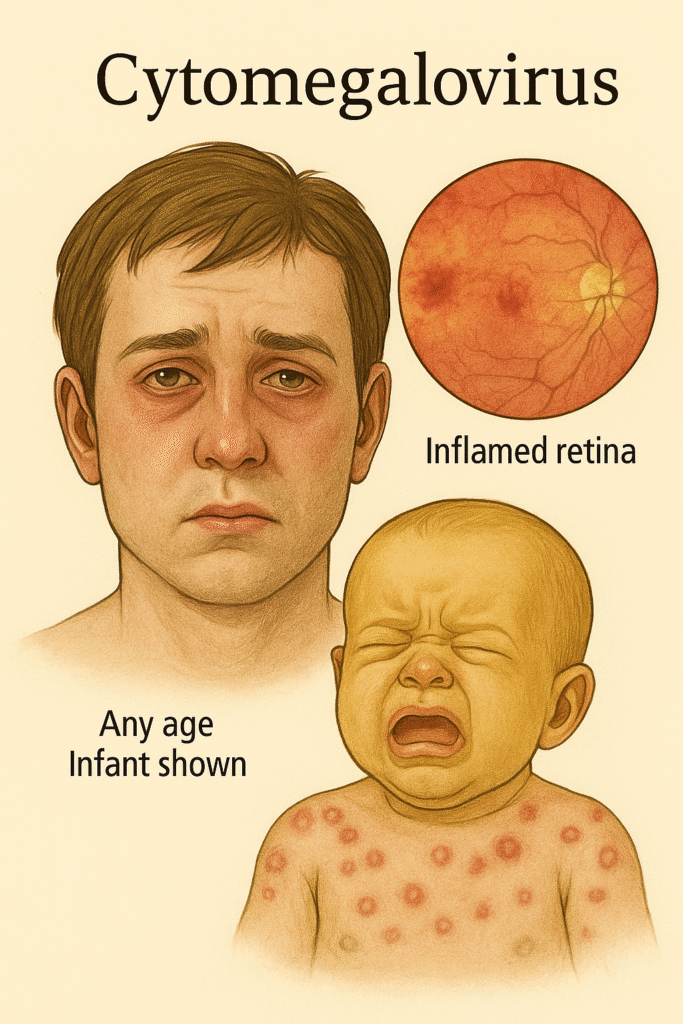
Clinical Features
In Fetuses:
- Infection during first trimester → Congenital abnormalities
- Microcephaly, seizures, deafness, jaundice, hepatosplenomegaly, purpura (blueberry muffin lesion)
In Immunocompetent Individuals:
- Asymptomatic or mononucleosis-like illness (heterophil negative)
In Immunocompromised Patients:
- Pneumonitis, esophagitis, hepatitis, colitis, retinitis, anemia, thrombocytopenia
Latency and Immune Evasion
- CMV becomes latent in monocytes
- Prevents MHC class I display → Avoids cytotoxic T cells
- Encodes microRNAs and chemokine receptor mimics to inhibit immune response
- Suppresses T cell function → Causes immunosuppression
Laboratory Diagnosis
- PCR: Detects CMV DNA/RNA in fluids and tissues
- Culture: Shell vial culture method
- Microscopy: Shows enlarged cells with “owl’s eye” inclusion bodies
Human Herpesvirus 6 (HHV-6)
- Causes Roseola Infantum in children (6 months to 3 years)
- High fever followed by maculopapular rash on face and trunk
- Infects T and B lymphocytes
- Can reactivate in immunocompromised → pneumonia, encephalitis, hepatitis
- Common cause of encephalitis after stem cell transplantation
Human Herpesvirus 8 (HHV-8 / KSHV)
- Causes Kaposi’s sarcoma
- Also associated with:
- Body cavity-based lymphoma (in AIDS)
- Multicentric Castleman’s disease
- Transmission: Sexual contact, blood transfusion, organ transplantation, oral secretions
For more detailed information, visit authoritative sources:
Table of Contents
You may also Like: Chickenpox and Shingles: 7 Essential Facts You Must Know About VZV Infection