Drug excretion
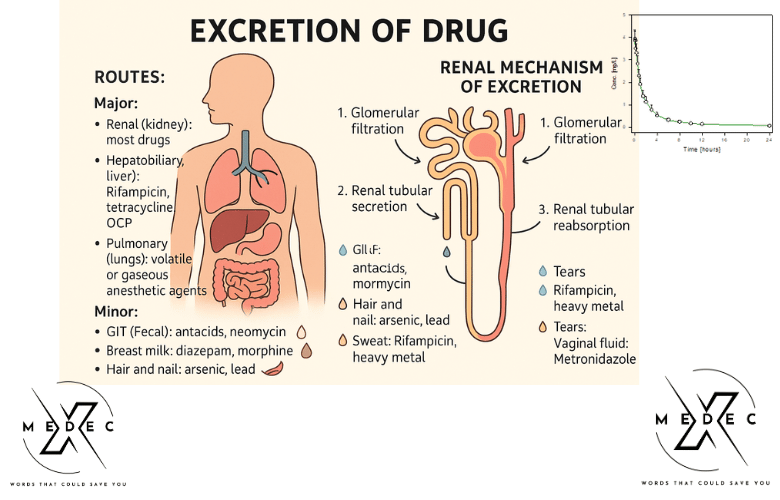
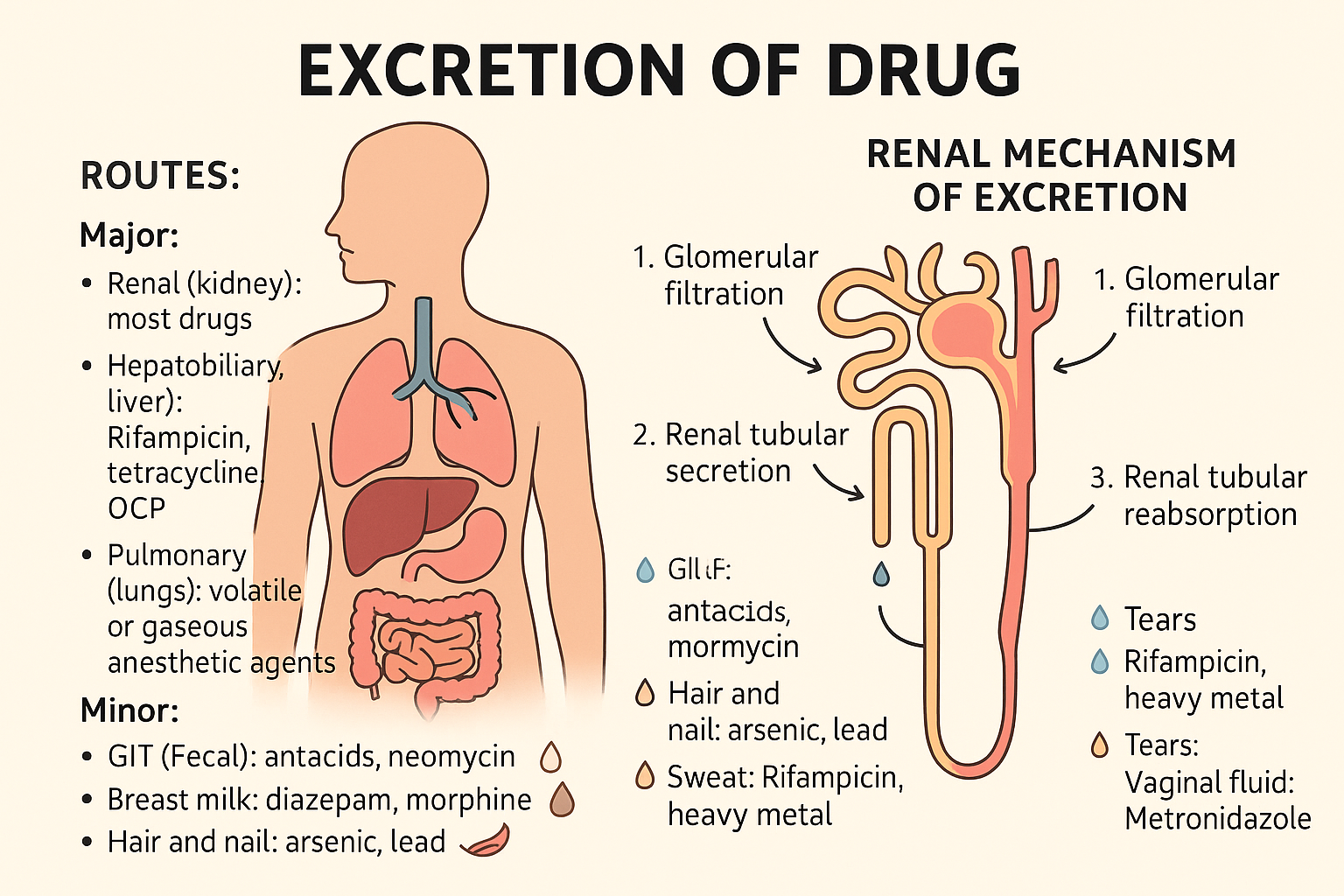
Drug excretion:
Removal of drugs from the body.
Routes:
Major:
- Renal (kidney): most drugs except protein bound drugs
- Hepatobiliary (liver): Rifampicin, tetracycline, OCP
- Pulmonary (lungs): volatile or gaseous anesthetics agents (halothane, nitrous oxide)
Minor:
- GIT (Fecal): Antacids, neomycin
- Breast milk: Diazepam, morphine
- Hair and nail: Arsenic, lead
- Saliva: Rifampicin, Metronidazole
- Sweat: Rifampicin, heavy metal
- Tears: Rifampicin
- Vaginal fluid: Metronidazole
Renal mechanism of excretion
- Consists of 3 mechanisms:
1. Glomerular filtration _ depends on GFR, plasma
- binding of drug, drug molecular wt.
2. Renal tubular secretion_ transfer drugs from plasma to tubular fluid through active transport by 2 systems, Organic acid transport (penicillin, probenecid), Organic base transport (thiazides, furosemide)
- Drugs using same active transport compete with each other. Probenecid and penicillin compete for same active site of carrier protein for secretion into renal tubule.
- Probenecid has more affinity for active site. It blocks the active transport of penicillin.
Probenecid is secreted into tubule and penicillin remains in plasma. So, action of penicillin is prolonged.
3. Renal tubular reabsorption_ depends on pK of drug & pH of tubular fluid
- If fluid is alkaline, acidic drugs ionise, less lipid
soluble, less reabsorption, more excretion
- But basic drugs are unionised, more lipid soluble, more reabsorption, less excretion
- Basic drugs are more rapidly excreted in acidic urine
- Acidic drugs are more rapidly excreted in alkaline urine
Significance
Useful in treatment of drug poisoning:
- Phenobarbital (weak acid) poisoning, Bicarbonate given, urine becomes alkaline, drug becomes ionized, decreased reabsorption, increased excretion/clearance
- Urinary alkalinisation is used to accelerate the excretion of salicylate in treating aspirin overdose
Cocaine (weak base) poisoning,
NH4Cl given, urine becomes acidic, drug becomes ionized, decreased reabsorption increased excretion/clearance
Factors that modify renal drug excretion
- Renal blood flow
- Lipid solubility of drug
- Urinary pH & ionization of drug: ionized form is not reabsorbed. Acidic drug in acidic urine is non-ionized, so is reabsorbed
- Drug interaction: active secretion
- Age & disease conditions: Many drugs are removed by renal excretion & cause toxicity in elderly & patients with renal disease.
- Urine flow rate
Half life:
It is the time taken by a drug to decline to half of its original value
t 1/2 = 0.693 x Vd(volume of distribution)
Clearance
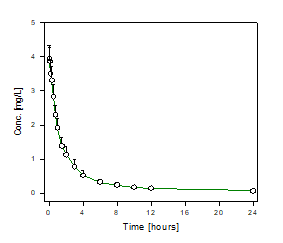
eg: Benzylpenicillin (30 min), Paracetamol (2 hrs)
It takes about 5 half lives for total elimination of a drug
Importance of half life
- Useful in designing drug dosage schedule
- To predict duration of action
- To handle a case of overdose
- To determine the time to achieve steady state concentration
Drug Kinetics: First Order, Zero Order, Enterohepatic Circulation
Order of Processes/Kinetics
First-Order Kinetics
- A constant fraction of the drug is transported/metabolized per unit time.
- The rates of absorption, distribution, metabolism, and excretion are directly proportional to the concentration of the drug.
- Rate of elimination ∝ Amount of drug
- Half-life is constant
- Examples: Most drugs
Zero-Order Kinetics
- A constant amount of the drug is transported/metabolized per unit time.
- Rates of absorption, distribution, metabolism, and excretion are not directly proportional to the drug concentration.
- Half-life is not constant
- Examples: Aspirin (high dose), Ethanol, Phenytoin
Enterohepatic Circulation
Some drugs form conjugates with glucuronic acid in the liver. This glucuronide enters bile and then reaches the gut. The parent drug is released due to hydrolysis by intestinal enzymes and bacteria. It is then reabsorbed from the gut mucosa into the liver and reconjugates with glucuronic acid.
Importance:
- Increases plasma concentration and effect of drugs.
- Provides a backup pathway when renal function is impaired.
- Examples: Rifampicin, Oral contraceptives, Tetracycline
Steady-State Plasma Concentration of Drug
Following continuous IV infusion, drug plasma concentration increases until steady-state concentration (Css) is achieved, where rate of input equals rate of output.
- Css → Input = Output
- Steady state is typically reached after 3 to 5 half-lives:
- 1st t½ → 50%
- 2nd t½ → 75%
- 3rd t½ → 87.5%
- 4th t½ → 93.75%
- 5th t½ → 96.875%
- Complete elimination of drug takes about 3–5 half-lives.
- If the half-life is known, time to reach steady state can be calculated.
Steady-State Concentration Formula:
Css = Ro / (Vd × ke)
Where:
Css = Steady-state concentration
Ro = Infusion rate (mg/min)
Vd = Volume of distribution
ke = First-order elimination rate constant
Loading Dose
A single or few quickly repeated doses given at the beginning to attain target concentration rapidly.
Importance:
- Achieves steady state quickly by starting with a larger dose.
- Used for drugs with long half-life or in emergencies.
- Example: Lidocaine in arrhythmia
Maintenance Dose
Dose that is repeated at specific intervals after achieving steady-state concentration to maintain drug levels by balancing elimination.
Understand how different drugs are absorbed, distributed, metabolized, and excreted.
Table of Contents
You may also like