Pharmacodynamic of drug
Pharmacodynamic:
It is a branch of pharmacology that deals with the mechanism of action and pharmacological effects of a drug.
Four targets of drug action (target proteins):
- Receptors (cholinergic and adrenergic receptors)
- Ion Channels (Ca⁺ channel, K⁺ channel)
- Enzymes (cholinesterase, cyclo-oxygenase)
- Carriers (transporters in renal tubular cells)
Types
- According to location
Membrane receptor: cholinergic receptors
Cytoplasmic receptor: steroid receptors
Nuclear receptor: thyroid receptors
- According to activity
Active receptor: adrenoceptors (1-2%)
Silent receptor: plasma protein
Spare receptor: (98%)
Receptor mediated mechanism:
Type 1 (Direct ligand gated ion channel): Drug binds directly with ligand gated ion channel, regulation of ions across cell membrane occurs (fast synaptic transmission) e.g:
Benzodiazepine receptor: Chloride channel opens, hyperpolarisation occurs, producing an inhibitory effect
Nicotinic receptor: Sodium channel opens, depolarisation occurs, producing an excitatory effect
Type 2 (G-protein coupled receptor system):
Receptors are linked to enzyme/ion channels by G-protein. Ligands bind to the receptor, G-protein is activated, which changes the activity of effector enzymes/ion channels, then via the second messenger, cellular effects are produced
- Adrenoceptors
- Muscarinic receptors
Second messenger: Chemical substances produced when a ligand binds with G-protein coupled receptor, via which cellular effect is produced. E.g: cAMP, IP₃, DAG
Type 3 (Enzymatic receptors): drug binds with
Transmembrane receptor (bound to protein tyrosine kinase), confirmational change occurs, activated tyrosine kinase produces phosphorylation of other cellular proteins to produce effect of drug.
- tyrosine kinase receptor
Type 4 (Intracellular receptors): drug binds with receptor in cytosol, enters nucleus and regulate gene expression for protein synthesis to produce effect of drug
- steroid receptors
Non-specific mechanisms:
- Enzyme mediated_ enzyme inhibition by
- physostigmine, neostigmine, OPC, NSAID, ACEi
- Alteration of metabolic process of cell_ penicillin
- Alteration of ion transport_ diuretics
- Chemical interaction_ neutralisation, chelation
- Alteration of physiochemical property of cells_
- laxatives
Dose-Response Relationship
- Affinity_ Tendency of a drug to bind with a receptor
- Efficacy_ Ability of a drug to bind to a receptor and produce a pharmacological effect
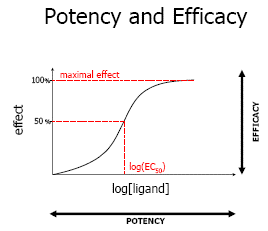
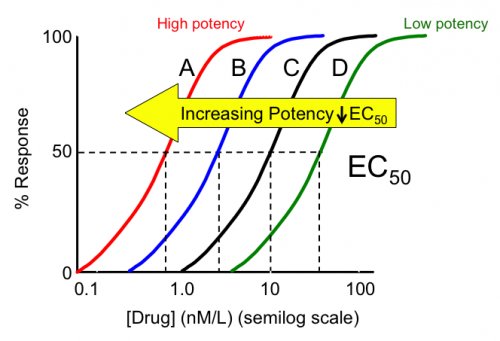
- Potency_ The dose of drug required to produce 50% of its maximal effect
- Agonist_ A drug that binds with receptor & activates it to produce a pharmacological effect. Eg: salbutamol (β receptor agonist), adrenaline (α and β receptor agonist)
- Partial agonist_ A drug that has affinity for receptor but with weak activity. Eg: pindolol (β receptor agonist)
- Inverse agonist_ A drug that has affinity for receptor but produces opposite effect to that of an agonist.
Eg: ß carboline (benzodiazepine receptor)
- Antagonist_ A drug that has affinity for receptor but blocks the receptor and produces no effect.
Eg: propranolol (β receptor antagonist)
- Effective dose_ dose which produces desired pharmacological effect
- ED50 (median effective dose): dose which produces desired pharmacological effect in 50% of experimental animals or individuals
- EDmax: dose of drug which produces maximum pharmacological effect
- Toxic dose: Excess amount of drug that produce toxic effect
- TD50 (median toxic dose): Amount of drug that produces toxic effect in 50% of individuals
- Lethal dose: Amount of drug that produces death in certain number of experimental animals
- Fatal dose: Amount of drug that produces death in 100% experimental animals
Therapeutic index: Ratio between median toxic dose and median effective dose
TI = TD50/ED50
Importance of TI
- Reflects the safety margin of drug_ high TI, more safe
- For safe application of drug TI must be > 1
Drugs with low TI : barbiturates, anticancer drugs
Drugs with high TI _ diazepam, antacid
Therapeutic window_ Dose of a drug between minimum effective concentration and minimum toxic concentration, where treatment is safest & most effective.
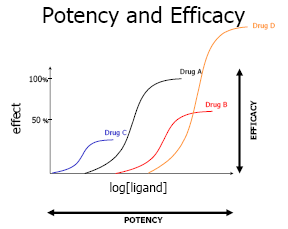
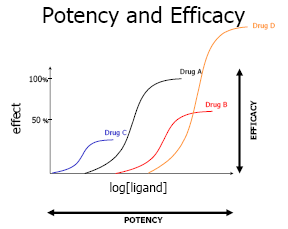
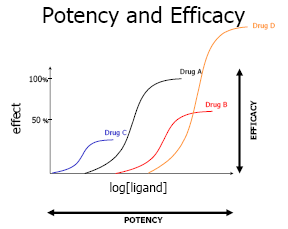
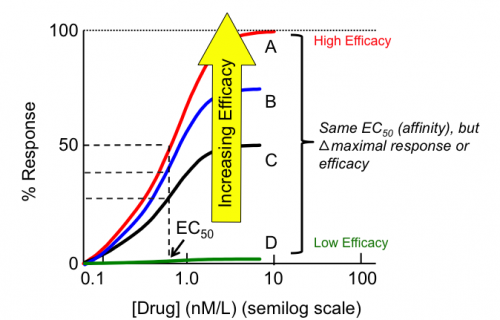
Dose & response relationship curves:
- Graded dose response relationship curve_
- Graph which shows the relation between dose of a drug with the magnitude of drug response sigmoid curve (log graph)
- As dose increases, increase in drug response is continuous and gradual
- Ceiling effect: maximum effect of drug
- Potency and efficacy can be compared
- Quantal dose response curve: all or none response (anaesthetics)
| GRADED DOSE RESPONSE CURVE |
QUANTAL DOSE-RESPONSE CURVE
Efficacy:
- determines clinical effectiveness of drug
- helps to select among drugs of same potency
Potency:
- determines the dose of the chosen drug
- affected by affinity and efficacy of drug
Pharmacodynamic Interaction
1. Synergism
- Summation / Addition
- Potentiation
Drug Synergism:
Synergism is when the action of one drug is facilitated or increased by another drug.
a) Addition:
Effect of drugs (A + B) = Effect of drug A + Effect of drug B
Example: 2 + 2 = 4
Beta-blocker + Thiazide diuretic → More antihypertensive effect
b) Potentiation:
Combined effect is greater than the individual effects of the drugs.
Effect of drug (A + B) > Effect of drug A + Effect of drug B
Example: 2 + 2 > 4
Trimethoprim + Sulfonamide → Cotrimoxazole
2. Antagonism
- Chemical antagonism
- Physiological antagonism
- Pharmacological antagonism
Drug Antagonism:
When the effect of one drug is reduced or blocked by the effect of another drug.
1. Chemical Antagonism
Two drugs react by chemical reaction.
Gastric HCl + Antacid → Chemical neutralization of gastric acid
Heparin + Protamine sulfate → Chemical neutralization of heparin
2. Physiological Antagonism
When one drug antagonizes the action of another by acting on a different receptor of the same physiological system.
Histamine (causes bronchoconstriction via histamine receptor) in bronchus
vs.
Adrenaline (causes bronchodilation via β₂ receptor) in bronchus
3. Pharmacological Antagonism
When one drug blocks the action of another by acting on the same receptor.
Types:
- Competitive Antagonism
- Binds to the same receptor
- Chemically resembles the agonist
- Produces a parallel right shift of the Dose-Response Curve (DRC) with increasing dose of agonist
- Intensity depends on the concentration of both agonist and antagonist
- Examples: Acetylcholine and Atropine, Morphine and Naloxone
- Non-Competitive Antagonism
- Binds to a different site
- No chemical resemblance
- Suppresses the maximum response
- Intensity depends only on the concentration of the antagonist
- Examples: Diazepam and Bicuculline
Table of Contents
Understand key concepts of pharmacodynamic interactions such as synergism, potentiation, and antagonism — including competitive and non-competitive mechanisms. Learn more from NCBI’s Pharmacology Reference.
You may also like the Pharmacokinetics topic: