Hernia Symptoms and Treatment: A Complete Guide to Types, Causes, Surgery, and Prevention
Hernia: Complete Guide
Hernia: A Complete and Comprehensive Guide
Definition of Hernia
A hernia is the abnormal protrusion of an organ or tissue through a weakened area in the muscle or connective tissue that normally contains it. It typically appears as a visible bulge, which may increase in size with activities such as coughing, straining, or lifting heavy objects.
Etiology of Hernia
Hernias can develop due to multiple factors, including:
- Congenital weakness of the abdominal wall
- Increased intra-abdominal pressure
- Previous surgical incisions (incisional hernia)
- Natural aging process leading to muscle weakening
Risk Factors for Hernia
- Male gender (higher risk for inguinal hernias)
- Advanced age
- Chronic cough or respiratory diseases (e.g., COPD)
- Obesity
- Heavy lifting or strenuous physical activity
- Constipation or straining during bowel movements
- Prostate enlargement causing urinary straining
- Smoking (weakens connective tissue)
Aggravating Factors of Hernia
- Chronic Obstructive Pulmonary Disease (COPD): Persistent coughing increases intra-abdominal pressure, weakening the abdominal wall.
- Weight Lifting: Repeated heavy lifting causes strain on the abdominal muscles, promoting hernia formation.
- Constipation: Straining during defecation repeatedly increases abdominal pressure.
- Benign Prostatic Hyperplasia (BPH): Chronic straining during urination due to prostatic obstruction predisposes individuals to hernia.
Cardinal Features of Hernia
- Visible Cough Impulse: The hernia becomes more prominent when the patient coughs.
- Palpable Impulse: The hernia can often be felt moving during coughing or straining.
- Reducibility: The ability to push the hernia contents back into the abdomen.
- Pain or Discomfort: Especially during activities that increase intra-abdominal pressure.
Classification of Hernia
1. External Hernias
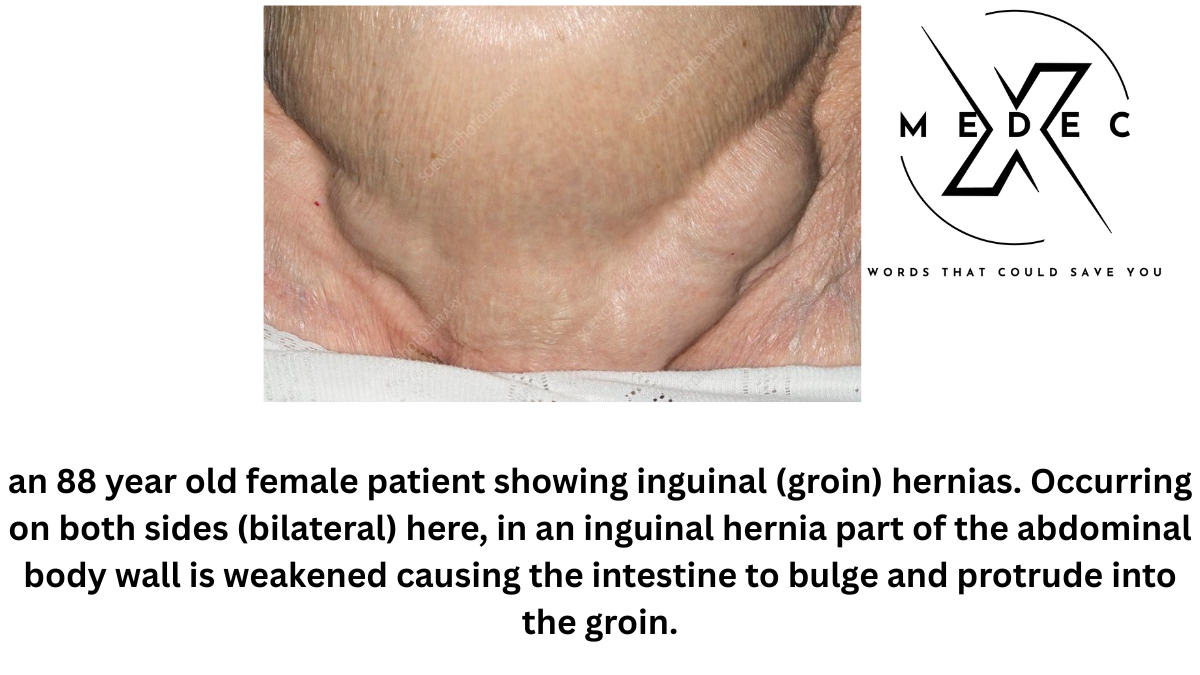
- Inguinal Hernia: Occurs in the groin area.
- Umbilical Hernia: Occurs near the umbilicus.
- Paraumbilical Hernia: Occurs adjacent to the umbilicus.
- Epigastric Hernia: Occurs in the upper midline of the abdomen.
- Incisional Hernia: Occurs at the site of previous surgical incisions.
- Lumbar Hernia: Occurs in the lumbar (lower back) region.
2. Internal Hernias
- Esophageal Hiatus Hernia: Occurs at the diaphragm’s esophageal opening.
- Foramen of Morgagni Hernia: Anterior diaphragmatic defect.
- Bochdalek Hernia: Posterolateral diaphragmatic defect, often life-threatening in newborns due to respiratory distress.
- Spigelian Hernia: Occurs along the semilunar line near the level of the arcuate line.
- Obturator Hernia: Protrusion through the obturator foramen in the pelvis, commonly seen in elderly, thin women, often presents with Howship-Romberg sign (inner thigh pain).
Comparison of Hernia Types
| Hernia Type | Location | Common in | Key Feature |
|---|---|---|---|
| Indirect Inguinal Hernia | Lateral to inferior epigastric vessels | Young males | Can extend into the scrotum |
| Direct Inguinal Hernia | Medial to inferior epigastric vessels | Older males | Bulges through Hesselbach’s triangle |
| Femoral Hernia | Below the inguinal ligament | Women | High risk of strangulation |
| Umbilical Hernia | Near the navel | Infants and overweight adults | May resolve in children |
Inguinal Hernia Detailed Anatomy
Deep Inguinal Ring
- Shape: Inverted U-shaped opening.
- Location: Approximately 1.25 cm above the midpoint of the inguinal ligament.
Superficial Inguinal Ring
Formed by the external oblique aponeurosis. The fibers split to form a triangular opening with attachments to the symphysis pubis and the pubic tubercle.
Inguinal Canal
- Indirect Inguinal Hernia: Herniated viscera enter through the deep inguinal ring and pass through the inguinal canal, potentially reaching the scrotum.
- Direct Inguinal Hernia: Herniated viscera protrude medial to the inferior epigastric vessels, through the posterior wall of the canal.
Hesselbach’s Triangle (Direct Hernia Site)
- Medial: Lateral edge of the rectus abdominis muscle.
- Lateral: Inferior epigastric vessels.
- Inferior: Inguinal ligament.
If the hernia passes through Hesselbach’s triangle, it is a direct inguinal hernia. If the hernia passes lateral to the triangle, it is an indirect inguinal hernia.
Complete vs. Incomplete Hernia
- Complete Hernia: The hernial sac extends into the scrotum and may reach the bottom of the scrotal sac.
- Incomplete Hernia: The hernia does not descend into the scrotum.
Reducible vs. Irreducible Hernia
- Reducible: Hernia can be pushed back into the abdominal cavity.
- Irreducible (Incarcerated): Cannot be reduced; risk of strangulation exists.
- Strangulated Hernia: Blood supply to the herniated organ is compromised, leading to ischemia and potential tissue death.
Bubonocele
A bubonocele is a type of inguinal hernia confined to the inguinal canal and does not descend into the scrotum. It is considered an early-stage indirect inguinal hernia.
Clinical Examination of Hernia
- Inspect the groin area for visible bulges.
- Palpate for the hernia impulse during coughing.
- Check reducibility by gently pushing the hernia back.
- Assess tenderness or signs of strangulation such as severe pain, redness, and irreducibility.
- Identify the presence of bubonocele if applicable.
Surgical Management Inguinal Hernia
Preoperative Assessment
Evaluate for comorbidities such as COPD, BPH, chronic constipation, and cardiovascular risks. Optimize patient’s general health before surgery.
Herniotomy
- Incision: Oblique incision parallel to the inguinal ligament.
- Procedure:
- Identify the hernial sac.
- Carefully dissect the sac.
- Open the fundus of the sac.
- Reduce the herniated contents.
- Transfix the sac at its neck.
- Excise the redundant sac.
- Repair using:
- Bassini Method: Interrupted sutures to approximate the inguinal ligament to the conjoint tendon.
- Darning Method: Continuous non-absorbable sutures to strengthen the posterior wall.
- Mesh Repair: Preferred method for adults for tension-free reinforcement to reduce recurrence.
If Indirect Inguinal Hernia:
- Herniotomy
- Herniorrhaphy (repair of the posterior wall)
- Mesh repair (gold standard in adults)
If Direct Inguinal Hernia:
- Herniorrhaphy
- Mesh repair (strongly preferred for long-term success)
Modern Laparoscopic Options
- TAPP (Transabdominal Preperitoneal) Repair: Involves entering the peritoneal cavity and placing a mesh over the hernia defect.
- TEP (Totally Extraperitoneal) Repair: Avoids entry into the peritoneal cavity and places mesh in the preperitoneal space.
Postoperative Considerations
- Monitor for wound infection, recurrence, hematoma, and chronic groin pain.
- Encourage early mobilization to prevent complications like deep vein thrombosis.
- Advise patients to avoid heavy lifting, manage constipation, treat chronic cough, and stop smoking to prevent recurrence.
Complications of Untreated Hernia
- Increasing pain and discomfort
- Incarceration (irreducible hernia)
- Strangulation leading to tissue death
- Intestinal obstruction
- Potential life-threatening emergencies if left untreated
Prevention of Hernia
- Maintain a healthy weight
- Avoid heavy lifting or use proper lifting techniques
- Manage chronic cough and constipation
- Stop smoking to improve tissue strength
- Exercise regularly to strengthen abdominal muscles
Patient Education and Lifestyle Advice
- Seek medical advice if a new lump or swelling appears.
- Avoid strenuous activities until fully recovered post-surgery.
- Gradually return to physical activity as advised by the surgeon.
- Focus on diet and hydration to prevent constipation.
- Follow-up regularly to monitor for recurrence.
Conclusion
Hernia is a common but potentially serious surgical condition. A clear understanding of its types, risk factors, clinical features, and modern surgical techniques is essential for both healthcare providers and patients. Timely diagnosis, appropriate surgical repair, and preventive lifestyle changes are key to ensuring excellent long-term outcomes and minimizing the risk of recurrence.
Important Topic:
Strangulated Hernia
A strangulated hernia is a surgical emergency where the blood supply to the herniated organ is compromised. If not treated promptly, it can lead to tissue ischemia, necrosis, and life-threatening complications.
Causes
- Prolonged incarceration of the hernia.
- Swelling and venous congestion inside the hernia sac.
- Adhesions or tight hernia neck constricting the herniated organ.
Clinical Features
- Severe, constant abdominal pain.
- Tender, irreducible hernia swelling.
- Signs of bowel obstruction (vomiting, abdominal distension, constipation).
- Skin changes over the hernia (redness, warmth, possibly discoloration).
- Systemic signs like fever, tachycardia, and shock in advanced cases.
Diagnosis
- Clinical examination (irreducibility, tenderness, no cough impulse).
- Ultrasound or CT scan can confirm compromised blood flow.
Treatment
- Emergency surgical intervention is required.
- Herniotomy with resection of non-viable bowel if necessary.
- Mesh repair is typically avoided in contaminated fields.
Incisional Hernia
An incisional hernia occurs at the site of a previous surgical incision due to weakness or incomplete healing of the abdominal wall.
Causes
- Improper wound healing.
- Postoperative wound infection.
- Obesity and increased intra-abdominal pressure.
- Chronic coughing or straining.
- Multiple previous surgeries at the same site.
Clinical Features
- Bulging at or near a previous surgical scar.
- Pain or discomfort, especially when standing, lifting, or coughing.
- Reducibility in early stages, can become irreducible over time.
- Risk of obstruction or strangulation in advanced cases.
Diagnosis
- Physical examination showing a swelling at the scar site.
- Ultrasound or CT scan to assess the size and contents of the hernia.
Treatment
- Elective surgical repair (often with mesh reinforcement).
- Laparoscopic or open hernia repair depending on the case.
- Control of risk factors such as obesity and chronic cough.
Table of Contents
Further Reading and Trusted Resources
For more detailed medical information, patient-friendly explanations, and up-to-date research about Hernia Symptoms and Treatment: hernia symptoms, causes, and treatment options, you can visit the Mayo Clinic’s Hernia Overview. Mayo Clinic is a globally recognized, trusted healthcare organization that provides reliable and evidence-based health information.
You may also like The Alarming sign: when you need emergency appendix removal surgery














